News

Can Aspirin Prevent Bowel Cancer?
This clinical trial looked at whether a low dose of aspirin could help prevent bowel cancer from coming back after people had surgery for stage 1–3 tumours with specific mutations. Participants were grouped according to the tumour mutations present. Group A was the primary focus of the trial and included people who had a tumour with a common and specific mutation in the PIK3CA gene. Group B included people who had tumours with other mutations in the PIK3CA, PIK3R1, and PTEN genes. These genes are involved in the PI3K pathway - a cell signalling pathway that helps regulate cell growth. When faulty, it can contribute to uncontrolled cell division and tumour growth.
A total of 626 participants from four Nordic countries took part. Within 12 weeks of surgery, half of the participants received daily aspirin and half received a placebo, in addition to standard clinical treatment. After 3 years of follow-up, participants in Group A who took aspirin had a significantly lower rate of cancer recurrence (7.7%) compared to those who took the placebo (14.1%). A similar benefit was seen in Group B, though this was a secondary finding. Serious side effects were uncommon but slightly more frequent in the aspirin group compared to the placebo group. This trial provides evidence that taking aspirin may help reduce cancer recurrence in patients with certain tumour mutations. While more research is needed to determine the best dose and duration, and whether factors like weight and sex affect outcomes, aspirin could be a cost-effective and accessible additional treatment for bowel cancer.

Is the weight loss drug semaglutide (Wegovy/Ozempic) safe for people with inflammatory bowel diseases?
Semaglutide (branded as Wegovy/Ozempic) is a medication that has recently been approved for use in Aotearoa New Zealand as a weight loss treatment. It is a GLP-1 (glucagon-like-peptide-1) receptor agonist and was originally developed and utilised to manage type 2 diabetes. Semaglutide has also been shown to be effective for weight loss. It functions by binding to GLP-1 receptors, resulting in slowed gastric emptying and reduced appetite but it can also cause gastrointestinal adverse events in some people. This raises the question, is semaglutide safe for people with pre-existing gastrointestinal complications, such as those with inflammatory bowel diseases (IBD)?
Two recently published papers in the journal of Inflammatory Bowel Diseases sought to answer this question. First, to determine whether semaglutide was safe for those with IBD and second, whether semaglutide remained effective for weight loss in people with IBD.
The first study by Levine et al. showed that IBD patients taking semaglutide did not experience increased adverse IBD-related complications compared to those not taking the drug. The second paper by Desai et al. confirmed this result and further demonstrated that semaglutide remained as effective for weight-loss drug in obese people with IBD compared to a non-IBD obese population also taking the drug.
Together, these studies indicate that semaglutide is safe and effective for those with IBD, suggesting that using this treatment for co-morbidity with obesity could be considered without increased risk of IBD-related disease flares. However, it is always important to speak with your doctor before deciding whether a new medication is right for you.
To read about these studies in more detail follow the links below:
https://doi.org/10.1093/ibd/izae250

Healthy eating with IBD
We often hear from patients with inflammatory bowel disease (IBD) that they avoid fibre-rich foods such as vegetables, fruits, wholegrains, legumes, and lentils, fearing they’ll trigger gut symptoms. While reducing fibre may ease symptoms temporarily, avoiding it over long-term may not be ideal for overall health. Fibre-rich foods are essential not only for digestive health but also for providing key vitamins, minerals, polyphenols (antioxidants), and prebiotics that help maintain a balanced and healthy gut microbiome.
At the University of Otago, we conducted the Inflammatory Bowel Disease Lifestyle, Food and Exercise (IBDLiFE) study to explore how lifestyle education including heart-healthy eating and encouraging physical activity, could support people with IBD in remission. Participants in the intervention group received guidance from a research dietitian and were encouraged to eat more fibre-rich foods, choose healthier fats and proteins, and reduce discretionary foods like processed meats, chips.
Compared to the control group who only received pamphlets without dietitian input, the intervention group made several positive changes. Namely, they increased their fibre intake by an amount roughly equivalent to a slice of heavy grain bread or ¾ cup of cooked porridge, ate half a serving more fruit (the recommendation is at least two servings/day), reduced discretionary foods by nearly two servings, and lowered their daily sodium intake by 911 mg (approaching the recommended limit of 2000 mg/day). The feedback from the intervention group was also mostly positive
“…I’m more in tune with what foods my body reacts poorly to, and what it needs for a better bathroom experience…”
“…The study helped me try new things and add more variety to my diet…”
These findings suggest that with the right support from qualified professional such as a dietitian, people with IBD can make positive dietary changes without impacting their symptoms.
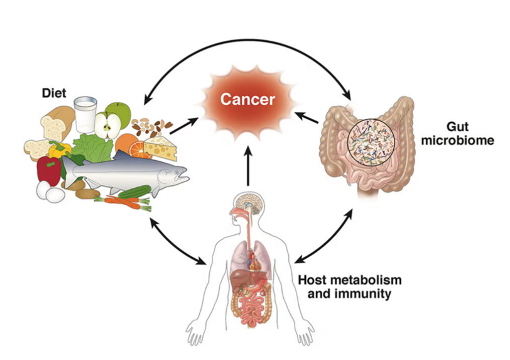
The Gut’s Hidden Power: How the microbiota can enhance colorectal cancer treatment.
Immunotherapy has limited effectiveness in microsatellite-stable colorectal cancer (MSS-CRC). Combining immunotherapy with radiotherapy has potential to enhance therapeutic benefit, but other contributing factors are often overlooked. The gut microbiota is a complex system of microbes able to improve or diminish CRC treatment. It is largely misunderstood how it does this and the extent of its impacts on CRC treatment outcomes. Using an MSS-CRC mouse model this study investigated the efficacy of immunotherapy and radiotherapy as well as both in combination, and specifically the effect of antibiotic treatment to diminish the microbiota on these therapies' efficacy. They found reduced efficacy with antibiotic treatment, and identified Bacteroides fragilis and propionate as crucial factors that enhance therapy. They propose adjunct therapy with Bacteroides-containing probiotics or supplemental propionate as a mechanism to enhance established CRC therapeutics. This highlights the importance of understanding the microbiota’s extent of contribution to CRC and other cancers.
Source: https://rdcu.be/eA7zf
A new shot at beating tough cancers!
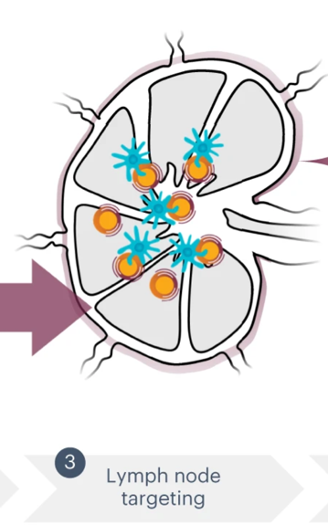
Locoregional therapies are cancer treatments that aim to directly target the tumour and surrounding tissues and are commonly used in colorectal cancer patients whose cancer has spread to the liver. Unfortunately, relapse is common following these treatments, and subsequent therapies often cannot cure the returning cancer. Recent research has shown that incorporating immunotherapies, which employ the immune system to fight cancer, with these tumour-targeting treatments may be a promising option for patients with liver metastasis. The success of these immunotherapies relies on the lymph nodes, which are vital for coordinating and sustaining the anti-cancer response.
Vaccines are a well-established way to prevent infections, but a new study has shown promising results that they could also extend the lives of colorectal cancer patients following locoregional therapies. A key problem with traditional vaccines is that they contain tend to have poor distribution to the lymph nodes. To give them the best chance of working as a cancer therapy, the researchers in this study created a vaccine that can ‘hitchhike’ on lipids in the blood to better reach the lymph nodes.
Their vaccine targets KRAS, a protein commonly mutated in cancer that is key to tumour’s ability to survive and grow. In the researchers’ first-in-human phase 1 clinical trial, this lymph-node targeting KRAS vaccine was given to five colorectal cancer patients who had residual disease following locoregional treatment. Following vaccination and over the course of monitoring, 60% of these patients had no detectable tumour DNA in their blood.
While this is an early-stage trial with a limited number of patients, the results suggest that lymph node-targeting vaccines could be a promising avenue for treating relapsing colorectal cancer which warrants further study. A phase 2 clinical trial is now underway to further explore these results.
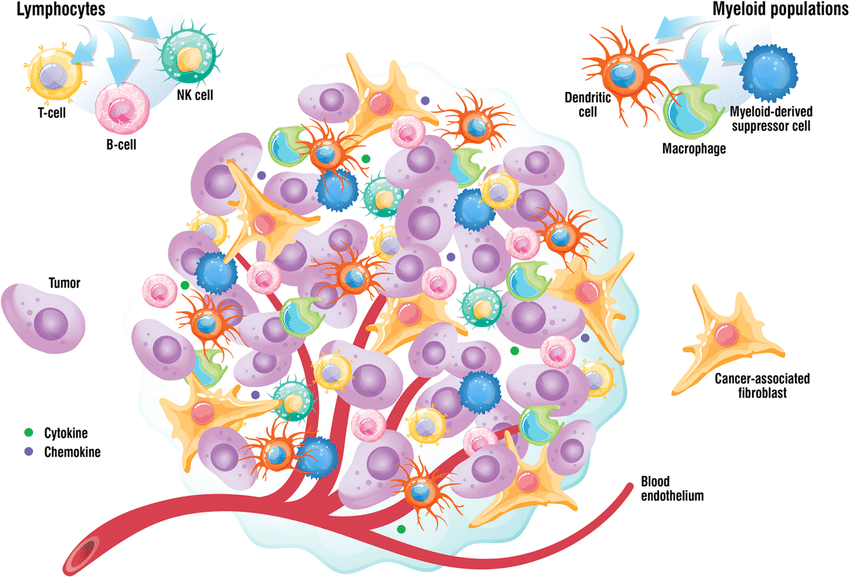
The gut microbiome and anti-PD1 immunotherapy
PD1, however a large portion of patients do not respond favourably.Previous studies have hinted that the gut microbiota influences how well these therapies work, with the abundance of certain bacteria being linked to clinical outcomes. However, the precise ways these gut microbes activate the immune response in distant tumours were not fully understoodTo investigate this, researchers collected faecal samples from cancer patients undergoing PD-1 blockade therapy, categorising them as responders or non-responders.They found that patients who responded had an enrichment of bacteria belonging to the Ruminococcaceae family. From these responders' samples, they successfully isolated a previously unknown bacterial strain, YB328, belonging to the genus Hominenteromicrobium.Results Summary:
- Faecal Microbiome Transplants from human responders enhanced the anti-tumour effects of PD-1 blockade in mice
- Administration of the YB328 alone did not inhibit tumour growth, but when combined with anti-PD-1 treatment, it significantly boosted anti-tumour efficacy across multiple mouse cancer models
- YB328 primarily activated CD103+CD11b− conventional dendritic cells (cDCs) in the gut which subsequently migrated to the tumour microenvironment to prime and activate CD8+ T cells
https://www.nature.com/articles/s41586-025-09249-8
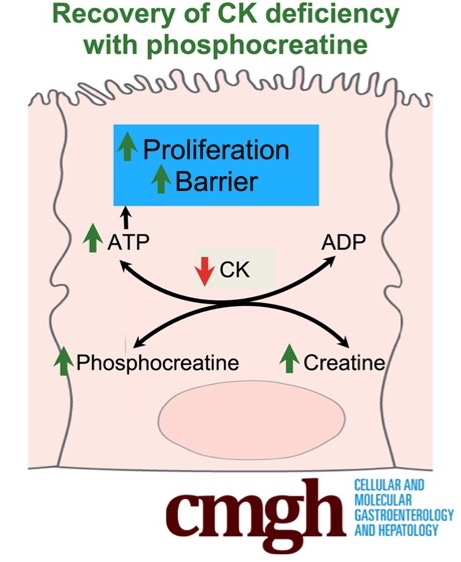
Restoring intestinal epithelial cell energy:
Creatine supplementation may help restore intestinal barrier function in inflammatory bowel disease:
Inflammatory bowel diseases (IBD) are characterised as the chronic inflammation of the digestive tract leading to the disruption of the intestinal epithelial cell lining. The intestinal epithelial cells have been shown to ineffectively use the energy from key molecules such as butyrate (a bacterial metabolite energy source) and creatine (an energy storer molecule) which restricts epithelial regeneration and barrier formation in IBD. In this study, the researchers used intestinal epithelial cell models (colonoids) derived from mice colonic biopsies to understand how the loss in the creatine kinase energy systems affects energy production and epithelial function.
The results from this study showed that a loss in creatine kinase led to an altered creatine energy pathway, energetic stress, and reduced intestinal epithelial cell function. An oral supplementation of phosphocreatine given to mice showed that this could potentially rescue the intestinal epithelial cell defects and restore the creatine kinase energy pathways.
This research indicates that creatine kinase supplementation may be a potential new strategy to help restore the creatine kinase energy levels to support intestinal epithelial cell barrier function in IBD.
Source: https://www.cmghjournal.org/article/S2352-345X(25)00098-0/fulltext
M.gnavus: a new biomarker for Spondyloarthritis in Crohn's disease patients
Spondyloarthritis is a common complication for Crohn’s disease patients, with approximately a third experiencing joint pain. It is thought to be caused by gut bacteria that escape the lumen when the intestinal barrier breaks down, triggering immune responses. Researchers from Weill Cornell Medicine recently investigated whether different types of bacteria are particularly responsible for these interactions and could be used as potential biomarkers.
To do this, they performed IgG sequencing on stool samples from 106 people (including CD patients without joint inflammation, those with peripheral spondyloarthritis, those with axial spondyloarthritis and healthy controls) and analysed the samples to determine which bacteria were associated with each group. The results showed that CD patients, with or without spondyloarthritis, had distinct and less diverse bacterial communities. These populations also differed between CD patients with peripheral or axial spondyloarthritis. Of these bacteria, Mediterraneibacter gnavus was highlighted as having elevated IgG in CD patients with both peripheral and axial spondyloarthritis. This IgG coating level also correlated with spondyloarthritis disease activity scores.
This research indicates that IgG reactivity against M. gnavus could serve as a biomarker to distinguish and monitor spondyloarthritis severity in Crohn’s disease patients, and may also be a potential target for future therapies. While these results are promising, it is important to note that additional studies are needed to confirm this potential biomarker in larger patient groups.

World IBD Day!

IT'S A WRAP
As the year comes to an end, I would like to take this opportunity to thank all who contributed to the Gut Health Network news items, it has been truly enlightening. We thank all our members for their continued support and wish all our patients and whānau a Merry Christmas and a Happy New Year. We will resume our website activities mid January, 2025. However, please feel free to reach us through contacts. We will be actively monitoring it over the holidays. Hope you all have a lovely break with friends and family. See you in 2025.
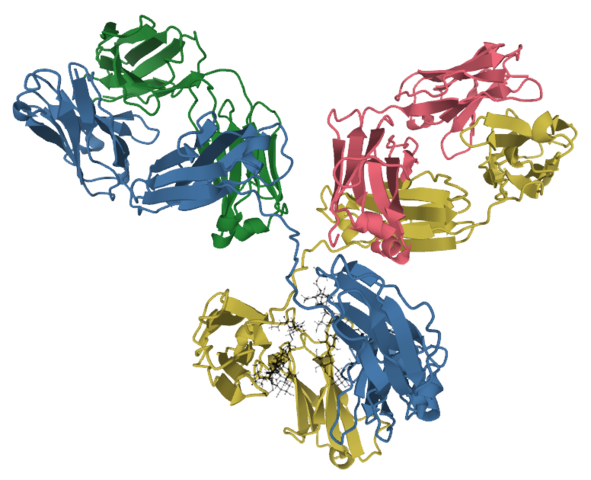
IgG glycosylation signatures predict future Crohn’s disease onset
Crohn’s disease is an inflammatory bowel disease that significantly affects quality of life. It is characterised by inflammation through the gut and the exact aetiology of the disease remains largely unknown. Research by Gaifem et al published in Nature Immunology investigated preclinical signs of Crohn’s disease in an effort to predict disease onset and perhaps prevent it.
By analysing serum samples up to 6 years prior to Crohn’s disease diagnosis, it was discovered that some circulating antibodies had a specific glycosylation signature in those eventually diagnosed with disease. This feature also correlated with increased levels of anti-microbial antibodies. Using a mouse model, it was determined that these antibodies reprogram innate immune cells to become more pro-inflammatory and increase susceptibility to colitis.
Altogether, this research indicates potential for a biomarker used to identify those with increased risk to progress to Crohn’s disease. Future research may determine ways to target these specific antibodies to prevent disease onset.
Source: https://www.nature.com/articles/s41590-024-01916-8
